Aligning provider incentives to change product use
April 6, 2013 at 11:05 AM Robert Kaminsky Leave a comment
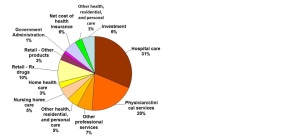
As we all know, US healthcare costs are greater than those in other parts of the world and rising. Health expenditures in the United States neared $2.6 trillion in 2010, over ten times the $256 billion spent in 1980. The rate of growth in recent years has slowed relative to the late 1990s and early 2000s, but is still expected to grow faster than national income over the foreseeable future. As the chart below shows, many segments of the healthcare system drive these costs, with most incurred in hospitals and by physicians.
Recently, MedSpan Research conducted a study by interviewing payers and providers about this challenge. We spoke with commercial, Medicare, managed Medicaid and state Medicaid payers. Respondents represented various functional areas, such as medical affairs, pharmacy and quality improvement. Providers represented integrated delivery systems, accountable care organizations, large medical groups and independent physician practices.
We explored:
- What aspects of healthcare costs should be addressed (e.g., administrative waste, unnecessary procedures, litigation)?
- What changes in the healthcare delivery system are required to achieve those objectives?
- What are the challenges with achieving success?
- What progress can be achieved over the next three years?
One of the foundational findings of the study is that successful management of healthcare costs requires an alignment of objectives and incentives among all key system players: payers, providers and patients. In today’s US healthcare system, most payers focus on managing short-term costs, providers drive patient health and satisfaction while protecting themselves from litigation and patients care only about their own outcomes and satisfaction. These differences in objectives lead to poor cost management and less than optimal outcomes.
Almost all payers and providers believe the system can achieve optimal outcomes at a lower cost of care. Aligned incentives are required to do so. One approach for aligning incentives is to develop compensation systems based on shared risks and rewards oriented towards agreed-upon objectives. Today’s dominant incentive systems, such as fee-for-service, DRG and per-diem rates, encourage resource utilization without incentives aimed at enhancing quality of care. Payers, especially government payers, are implementing provider compensation systems focused on enhancing the quality of care.
There are three types of provider compensation models currently in use:
- Utilization-based compensation — primarily fee for service
- Risk-shifting compensation — inpatient/outpatient prospective payment systems (PPS), capitation, per diem contracts and bundled/episodic payments
- Value-based compensation — Shared savings, risk sharing, pay-for-performance incentives
Today, more than three-quarters of all provider compensation is based on the utilization of healthcare resources, whether through fee-for-service or PPS. This contributes to the escalation of healthcare costs.
Today, value-based compensation is almost equally distributed among shared savings, risk sharing, and pay-for-performance incentives. Approximately three-quarters of all private payers utilize pay-for-performance incentives to some extent. While a much smaller percentage utilize shared savings and risk sharing models, the utilization of these models is expected to proliferate over the next three years. Almost two-thirds of all payers expect to utilize shared savings and risk sharing models for at least some of their providers by 2015.
This illustrates that payers and providers are open to experimenting with new compensation models over the next three years. Almost all payers suggest that it takes at least three years to determine the success of these models. Therefore, the adoption of these compensation models is expected to be measured.
Entry filed under: Healthcare Economics, Healthcare innovation, Healthcare Reform, Payer Reimbursement, Provider compensation. Tags: capitation, episodic payment, fee for service, healthcare costs, pay for performance, per-diem contracts, provider compensation, risk sharing, shared savings.

Trackback this post | Subscribe to the comments via RSS Feed